Vaccine and limitations
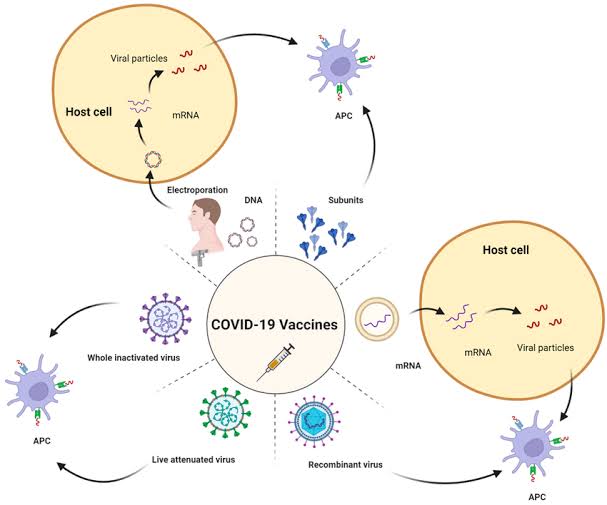
Good evening all, an effective vaccines can only be developed with an understanding of how viruses behave in the body—how they infect, spread, hide, and persist. The concept of viral tropism plays a key role in this. Viral tropism refers to the specific cells or tissues a virus prefers to infect.
This preference is based on whether the host cells have the internal machinery the virus needs to replicate and whether they express the appropriate receptors that the virus can bind to. For example, HIV targets CD4+ T cells because those cells have the CD4 receptor and co-receptors (like CCR5 or CXCR4) needed for viral entry.
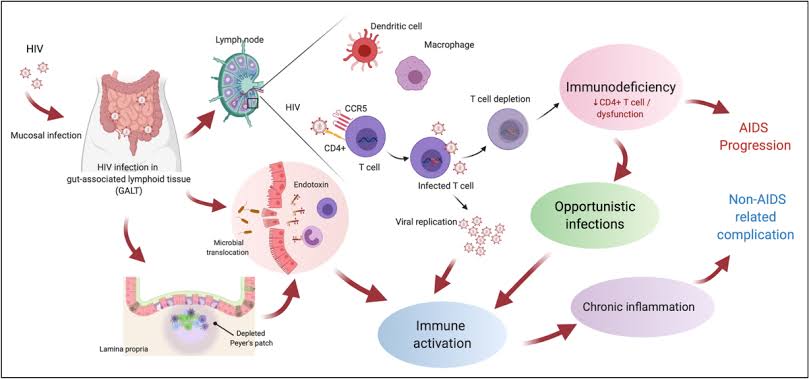
When developing vaccines, knowing which tissues the virus targets helps determine where the immune response should be strongest. For viruses that enter through the respiratory or genital tract, mucosal vaccines may be preferred. The course of a viral infection—whether it’s acute or chronic—depends on how the virus interacts with the immune system and whether it can complete its replication cycle quickly or linger in the host. The virus enters, multiplies, spreads, and is cleared by the immune system in an acute infection.

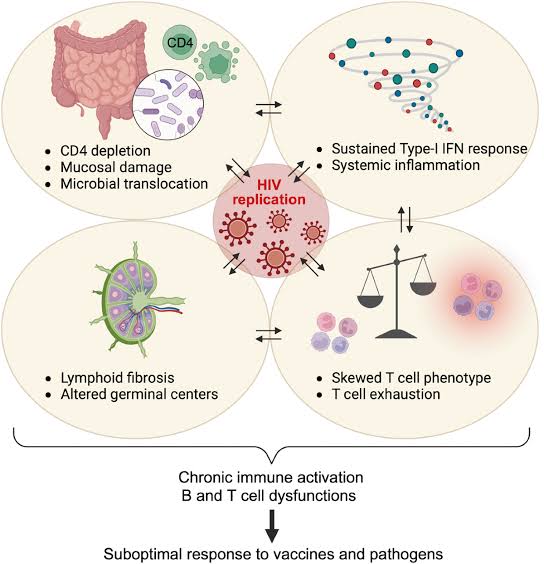
Vaccines for these types of viruses, such as measles or influenza, aim to induce strong, short-term immune protection that can prevent infection or limit its spread. On the other hand, vaccines make it much harder to control chronic infections like HIV, HBV, and herpesviruses because the viruses have evolved ways to stay in the body for life. Immune evasion strategies are utilized by many of these persistent viruses. HIV, for example, mutates rapidly, so the immune system can’t keep up with the changing virus. It also reduces the visibility of infected cells by downregulating MHC-I molecules, making it harder for cytotoxic T cells to recognize and destroy them. Proteins that resemble human cytokines like IL-10 are produced by some viruses, such as the Epstein-Barr virus (EBV) and the cytomegalovirus (CMV), which typically aid in reducing inflammation. These viral IL-10 homologs suppress the host immune response and create a favorable environment for the virus to persist without being attacked. Because an effective vaccine must not only stimulate an immune response but also overcome or bypass these viral countermeasures, this presents a significant challenge for vaccine design. HIV takes immune evasion a step further by hiding in what we call viral reservoirs. The virus integrates into the host DNA and remains silent in these groups of cells, mostly resting memory CD4+ T cells. Because it’s not actively replicating in these cells, the immune system and antiretroviral drugs can’t detect or remove it. This is the reason why HIV is so difficult to cure and why a traditional vaccine strategy—like the ones used for flu or measles—hasn’t worked yet. Any potential HIV vaccine must not only prevent infection but also stop the virus from establishing these hidden reservoirs in the first place.
The herpesviruses (like HSV, VZV, EBV) also persist in the body using latency. After the initial infection, they retreat into specific cells (like neurons or B cells) and remain dormant. Later, especially when the immune system is weakened, they can reactivate and cause symptoms again. The body never fully clears them. This latency and reactivation cycle makes vaccine development more complex. An ideal herpesvirus vaccine would need to prevent both the primary infection and the later reactivations—something current vaccines struggle to achieve.
Medical strategies like ART (antiretroviral therapy) and PrEP (pre-exposure prophylaxis) have provided essential tools for managing and preventing HIV. ART helps people living with HIV by reducing viral replication to undetectable levels, improving immune function, and preventing transmission. On the other hand, PrEP is used by HIV-negative but high-risk individuals. It works like a medical vaccine—taken regularly to block HIV before it can establish infection. These treatments provide insight into how a real preventive vaccine might work: by stopping infection at the earliest possible stage, even before the virus can reach its reservoir sites.
The difficulties posed by viruses such as HIV and herpesviruses extend beyond simply eradicating the initial infection. Their ability to hide, suppress the immune system, and reappear later in life forces us to think more broadly about what a vaccine must do. It’s not just about triggering antibodies—it’s about long-term cellular immunity, immune memory, and overcoming viral strategies like latency, immune suppression, and tissue-specific hiding. Understanding these viral behaviors is key to creating the next generation of vaccines that go beyond prevention and move toward control—or even cure—of chronic viral infections.
This is my entry on the ongoing content #scifimultiverse topic science of vaccines.
Thank you for stopping by my blog; I appreciate your comments, support and upvotes. Do have a lovely evening.
Do well to source your images.
Also Kindly Share your entry link in our discord, and tag three people you supported.
Alright
Do well to add the link or source of the pictures used as they are not yours.
You must be into medicine to have come up with this deep knowledge.
Nice one bro
Wow, I learnt alot from reading this post.
Thanks for sharing, this is highly educative.